Palliative care guidelines
Guidelines for palliative care
Because it plays such a key role, it’s important to establish some guidelines for palliative care.
Coming to the end of life can be a difficult time for everyone involved. There are lots of important decisions to make for the individual’s care and also what will happen after they die. As well as the practical elements of palliative care, a large part of this process is providing the right emotional and psychological support for the person receiving care and their loved ones.
Palliative care guidelines are used in order to limit discomfort and ensure that the care is centred around the individual, with clear communication between health care professionals, family members, carers and the person receiving care.

What is the palliative care guideline?

The palliative care guideline outlines how a person should be cared for in their last weeks.
Created by the National Institute for Health and Care Excellence (NICE), the palliative care guideline details how someone within the last few days of their life should be cared for.
The focus of the guideline is very much about maintaining the dignity and comfort of the individual and involving them as much as possible with their care plans.
The guideline is centred around:
Planning care
Planning end-of-life care with the individual, their family and healthcare professionals
End-of-life support
Recognising when someone is in the last days of their life and requires more complex care
Comfort
Ensuring the person in question can remain comfortable – physically and emotionally
Medication
How to manage and administer the patient’s medication and what dosage to apply

Planning care
Where possible, it is important that the individual is involved with their end-of-life care plans. They should be included in all conversations regarding what will happen, and their wishes should be adhered to – for example, if they want to die at home without any further medical treatment or if they have particular religious requests.
If a person is unable to make these decisions due to capacity, their Power of Attorney should do this on their behalf.
End-of-life support
If someone has a terminal illness and begins to decline, they should be closely monitored for symptoms that show they are in the last days of their life to ensure they’re always receiving the right type and level of support, or are at least able to make an informed decision.
There should be daily assessments to determine whether their condition has worsened or improved. If they are deemed to be at the end of their life, this should be fully explained to both the individual and their loved ones. Sharing all or limited details is at the discretion of the individual and their care team.

Staying comfortable
There are a variety of symptoms that should be closely monitored during end-of-life care.
In order to ensure maximum comfort and dignity in an individual’s final months and weeks, there are a number of symptoms that should be addressed and steps that should be taken proactively. They are:
Pain
Pain levels should be limited as much as possible and treated with the most appropriate pain killers or relief to ensure a comfortable end of life
Breathlessness
This can be related to the individual’s primary health condition, or as a side effect. It should be managed effectively with pain relief or appropriate treatment.
Nausea and vomiting
Usually a side effect of treatment or related to their primary condition. Medication can be used to help or may have to be reduced if it’s causing nausea and vomiting.
Anxiety and delirium
These can be common for those in the last days or hours of their life, and can be treated with medication or reduced by the comfort of having familiar loved ones nearby
Hydration
If wanted, you can have support with drinking or a fluid drip if swallowing is difficult. Those who are unable to swallow can use oral gels and saliva replacements.
Constipation
When someone is living with a terminal illness, their eating habits, fluid intake, mobility and medication may change. These can all contribute to constipation.
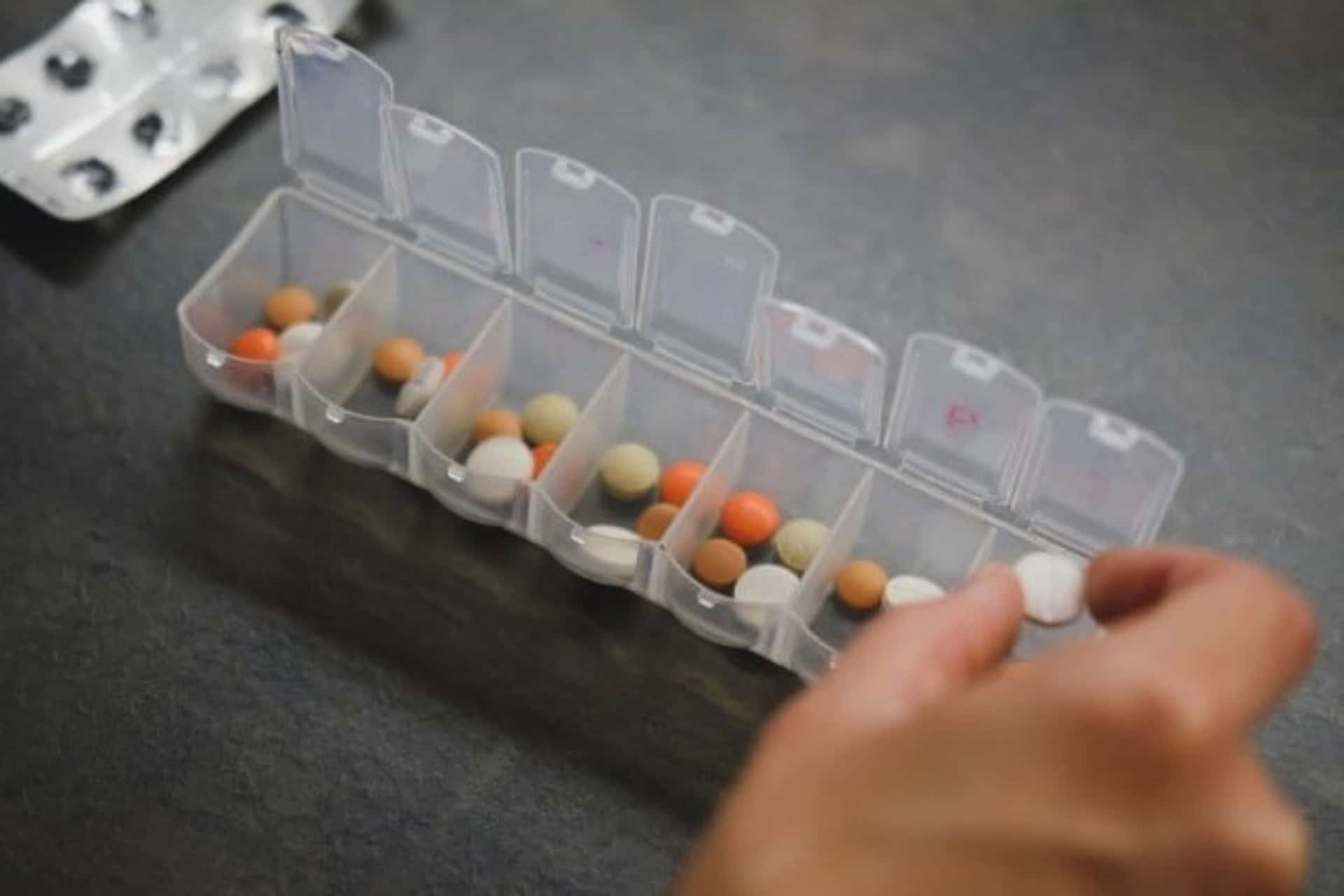
Medication
The person’s existing medication, any new medication required and how medicine is administered should all be considered for end-of-life care.
For those receiving care at home, there may be ‘just in case’ medication that is provided in advance of their symptoms worsening. These can be accessed quickly and limit their discomfort should they require extra medication at a later stage of their care.
You can read the full palliative care guideline here:
What is NICE and what do they do?
The National Institute for Health and Care Excellence (NICE) was created in 1999 as a national body dedicated to improving health and social care services across the UK.
They create evidence-based recommendations and guidelines for healthcare workers and practitioners to carry out the very best care, including within the NHS and private care services. They are committed to the highest quality standards across health and care services, carrying out research and working closely with the government, GP surgeries, hospitals and local authorities.
You can find out more about NICE here:
Replacing the Liverpool Care Pathway
The Liverpool Care Pathway (LCP) was a set of guidelines created during the late 90s aimed at providing the best quality end-of-life care for those in their final days and hours of life. It was designed to ensure that death was as dignified and pain-free as possible, and invasive treatment was stopped if it would not prevent death. It was adopted by many hospitals and care settings in the UK, and at the time was widely regarded as best practice for end-of-life care.
After complaints and controversy surrounding the LCP, including national media attention, the LCP was dissolved in 2015 and new palliative care guidelines were created by NICE to combat the concerns raised. They addressed the involvement of the individual and their family, as well as additional healthcare professionals as to when end-of-life care should commence.

The LCP included points such as:
Necessary treatment
Considering whether certain treatments were needed in a person’s final hours, such as taking blood pressure readings
Fluid support
Deciding if fluids should still be given, regardless of whether the individual is able to eat or drink or not
Comfort
Ensuring comfort, including their position in bed, breathing help and mouth care for over or under production of saliva
Emotional well-being
The emotional well-being of the individual; for example, fulfilling religious needs or having family members present
How we can help

Here at Helping Hands, we know how difficult this time can be for all involved.
If you or a loved one has a life-limiting condition or chronic illness and you’d like to discuss your future plans for care at home, you can talk to our dedicated customer care team who will find out more about your requirements and arrange a consultation with a care manager local to you.
We also offer emergency care if you are reaching the last few weeks or days of your life and would like to pass away at home. If you require urgent support, we can arrange for care to commence within 24 hours of your initial enquiry.
How to arrange palliative care
We aim to make it easy to arrange the support you want so that we can focus on what really matters: your care needs. Speak to our team today to begin your journey.
Speak to our team
Call our team of experts to talk through your options and any questions you may have
Free home care assessment
Your local Helping Hands manager will visit you to discuss your care requirements
Find your carer
We’ll help to match you with a carer who meets your preferences and has the right skills
Page reviewed by Carole Kerton-Church, Regional Clinical Lead, on November 8, 2021.
